Background:Uterine fibroids, also called leiomyomas, are diagnosed in over two-third of females of reproductive age; about a quarter warrant treatment. Venous thromboembolism (VTE) is a challenging complication in patients with fibroids due to the increased risk of bleeding with anticoagulation, especially in the setting of associated menorrhagia. The incidence of deep vein thrombosis (DVT) is increased with higher uterine weight which may be related to the extrinsic venous compression of the iliac veins or the inferior vena cava. However, there is reported discordance between the site of uterine fibroid and the site of the DVT along with pulmonary embolism (PE) without evidence of lower extremity DVT suggesting an underlying hypercoagulable state that is more complex than mere hormonal and mechanical factors. Data regarding VTE in patients with uterine fibroids in the US is sparse and is limited to case reports. We performed a retrospective case control study to describe the rate and associated risk factors of VTE in patients with uterine fibroids.
Objectives:Evaluate the incidence of VTE events in patients with uterine fibroids and explore trends and associations.
Methods:A retrospective chart review of patients at our single, academic, DC metropolitan hospital was conducted. Patients were identified using electronic medical records via ICD-10 codes. Those seen as an inpatient or outpatient in our tertiary care fibroid center with a new diagnosis of uterine fibroids between January 1, 2015, and December 31, 2019 were included and compared to age matched controls of patients with uterine fibroids without VTE in a 1:2 ratio. Statistical analysis was reported as means and medians for descriptive data. Pearson's correlation was performed to determine associations.
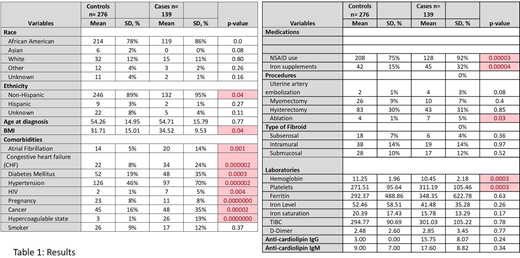
Results:A total of 6095 patients were diagnosed with uterine fibroids in 5 years, of which 2.2% (n=139) were found to have VTE after the diagnosis of uterine fibroid was made (see table 1). Of the patients with VTE, 88 had DVTs,63 had PE and 12 developed both DVT and PE. The mean age at diagnosis of VTE was 54 (SD=14.95) years. The majority of the patients in the VTE group were African Americans (86%) and mean BMI was 34.52 (SD =9.53), of which about 2/3 were obese or morbidly obese. Average weight of fibroid(s) for those who underwent surgical resection who had available records was noted to be 321 grams (n=11). Data regarding anticoagulation was available for 78% of the patients; the anticoagulant of choice being enoxaparin in 59%, warfarin in 9% and DOACs in 10% of the patients. Two Hundred and thirty-six age matched controls were identified. Statistically significant associations with BMI, race and comorbidities (including atrial fibrillation, congestive heart failure, diabetes, hypertension, HIV, pregnancy and cancer) were found in cases when compared to the control population. Furthermore, cases were found to have a lower mean hemoglobin (10.4 mg/dL) and higher platelet count (311,000/microL) which were statistically significant (p=0.0003). The use of non-steroidal anti-inflammatory drugs and iron supplementation was significantly more in cases than controls. D-dimer and ferritin levels seemed to trend higher and iron saturation lower in cases than controls but were not found to be statistically significant.
Conclusions:VTE was found in 2.2% of patients with uterine fibroids, which is higher than the reported VTE incidence of 1-2 per 1000 in the general population. A significant association was found with race, which is consistent with literature that suggests African American patients have a higher rate of incident VTE and also comorbid conditions. Women with low hemoglobin and higher platelet count were more likely to experience VTE. The next steps include understanding more associations, laboratory and clinical, that will assist in risk stratification and tailoring management. Future prospective studies to recognize biomarkers that contribute the hypercoagulable state of uterine fibroids is warranted.
Morozov:Medtronic:Consultancy;Lumenis:Speakers Bureau;AbbVie:Speakers Bureau.Fitzpatrick:Pfizer:Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.